Bullosis diabeticorum – una lesión poco común
Márcio Luís Duarte1,2*, Thaiza Alonso Simal3, Lucas Ribeiro dos Santos4, André de Queiroz Pereira da Silva2, José Luiz Masson de Almeida Prado2.
Bullosis diabeticorum – an uncommon lesion
1 Mestre em Saúde Baseada em
Evidências pela UNIFESP, São Paulo,
São Paulo, Brasil.
2 Radiologista do setor de Radiologia
Musculoesquelética da WEBIMAGEM,
São Paulo, São Paulo, Brasil.
3 Dermatologista e Mestre pela
UNIFESP, São Paulo, São Paulo, Brasil
4 Professor e Endocrinologista da
Faculdade de Ciência Médicas de
Santos, Santos, São Paulo, Brasil.
*Correspondencia: Márcio Luís Duarte /
marcioluisduarte@gmail.com
WEBIMAGEM, Avenida Marquês de
São Vicente 446, São Paulo, São Paulo,
Brasil. CEP: 01139-020.
Apoyo financiero: no hay.
Recibido: 12-08-2019
Aceptado: 22-10-2019
Resumen: Introducción: El bullosis diabeticorum forma parte del espectro de manifestaciones cutáneas de la diabetes mellitus, descrito por Kramer en 1930 y nombrado como bullosis diabeticorum por Cantwell y Martz. Es una enfermedad conocida, pero bastante rara (0.5 a 2% de la población diabética) siendo dos veces más común en hombres. Es una lesión espontánea y no está relacionada con trauma o causa fisiológica evidente, como infección, 3 que no causa dolor o se asocia a signos flogísticos. Se asocia principalmente a las extremidades, pudiendo ser una lesión única o múltiples lesiones. Puede ocurrir en la diabetes mellitus tipo 1 (DM1) y en el tipo 2. Las lesiones típicamente se curan espontáneamente de 2 a 6 semanas, pero pueden ocurrir en el mismo lugar nuevamente. El pronóstico es bueno, sin tratamiento específico necesario o seguimiento diagnóstico con biopsia. Se relata un caso de esta rara patología con documentación por resonancia magnética.
Palabras clave: Magnética, Pie diabético/diagnóstico, Resonancia, Vesícula/etiologia, Vesícula/ patologia.
Abstract: Bullosis diabeticorum is part of the spectrum of cutaneous manifestations of diabetes mellitus, described by Kramer in 1930 and named bullosis diabeticorum by Cantwell and Martz. It is a known disease, but quite rare (0.5 to 2% of the diabetic population) and is two times more common in men. Bullosis diabeticorum is a spontaneous lesion and not related to trauma or obvious physiological cause, such as infection that does not cause pain or is associated with inflammatory signs. Occurs at the limbs and may be single or multiple. It can occur in diabetes mellitus type 1 (DM1) and type 2, usually in the advanced stages. The lesions heal spontaneously typically in 2 to 6 weeks, but they may happen again on the same site. The prognosis is good with no need of special treatment or further diagnosis with biopsy. We report a case of this rare complication with magnetic resonance imaging.
Keywords: Blister/ etiology, Blister/pathology, Diabetic Foot/diagnosis, Magnetic Resonance
Bullosis diabeticorum is part of the spectrum of cutaneous manifestations of diabetes mellitus1,2, described by Kramer in 19301 and named bullosis diabeticorum by Cantwell and Martz3. It is a known disease, but quite rare (0,5 to 2% of the diabetic population)4, underdiagnosed in most cases2, and is two times more common in men4,5.
Bullosis diabeticorum is a spontaneous lesion, inflammatory and not related to trauma or obvious physiological cause, such as infection4 that does not cause pain or is associated with inflammatory signs4,6. The lesions appear rapidly, mainly in the acral region and limbs, varying in size and, may be single or multiple2,4. It can occur in diabetes mellitus type 1 (DM1) and type 2, usually in the advanced stages4.
We report a case of diabetes diabeticorum, a rare dermatologic lesion despite diabetes mellitus has a high incidence and prevalence worldwide, with a magnetic resonance imaging (MRI) study for evaluation of local infection and osteomyelitis.
Case report
A 74-year-old male patient refers a bullous lesion in the right hallux for one day, painlessly, without signs of inflammation. Refers type 2 diabetes mellitus (DM2) for ten years treated with diet. Started treatment with januvia and metformin two years ago. The glycaemia, even with drug treatment, remains at a level between 140-180 mg/dl. Denies surgeries and trauma.
The blister developed spontaneously with a diameter of 2.5 cm in the right hallux, without phlogistic signs, no erythematous base, apparently composed of dark serous contents. It was tense with negative Nikolsky sign. The patient had no other bullous cutaneous lesions around. The blister burst and spontaneously resolved without complications and without specific medication two days after physical examination (Figure 1).
A MRI of the right foot was performed to evaluate the possibility of infection in surrounding tissues and osteomyelitis. The MRI demonstrated a skin blister in the plantar aspect of the distal phalanx of the hallux (Figure 2) and a discreet peripheral contrast enhancement, without any signs of infection.
With anamnesis, physical examination and MRI, it was concluded that the lesion corresponded to a bullosis diabeticorum.

Figura 1. A) Blister in the right hallux, without phlogistic signs, no erythematous base, apparently composed of dark serous contents. (blue arrow). B) Ruptured blister without complications (blue arrow).
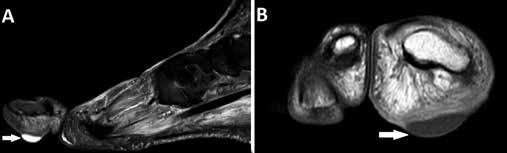
Figura 2. A) Sagittal T2 STIR MRI (A) and Coronal T1 weighted-image with contrast MRI (B) demonstrating skin blister in the hallux (white arrow), with discreet peripheral contrast enhancement, without any signs of infection (white arrow).
Discussion
The pathogenesis of the disease is not clearly understood2 – some theories relates metabolic disorders3 and also nephropathy7. In diabetic patients, there would be a greater tendency for blister forming mechanism for suction8. In other theories, microangiopathy explains the lesions with the histological finding of surface vessels hyalinosis9.
The liquid levels in the bullous would be explained by reepithelialization, commonly observed in this type of injury4.
The histological finding of injury shows a nonacanthotic subepidermal blister with liquid levels4. Histological diagnosis is necessary immunohistochemistry to differentiate from subepidermal blisters4,10.
The differential diagnosis includes:
- Bullous pemphigoid.2,11
- Chemical or electrical burns.2,11
- Drug-induced blister.2,6
- Epidermolysis bullosa.2,6
- Friction blister.2,11
- Porphyria cutanea tarda.11
- Pseudoporphyria.11
The lesions heal spontaneously typically in two to six weeks2,9, but they may happen again on the same site10. Secondary infection after rupture is a concern2 with MRI being useful to elucidate this complication, such as osteomyelitis12. The prognosis is good with no need of special treatment or further diagnosis with biopsy3.
We report a case of diabetes diabeticorum, a rare dermatologic lesion despite diabetes mellitus has a high incidence and prevalence worldwide, with a magnetic resonance imaging (MRI) study for evaluation of local infection and osteomyelitis, complications which were not confirmed by the imaging test.
Conclusion
We report a case of bullosis diabeticorum in the hallux
characterized by MRI. In cases where there is a bullous
lesion, bullosis diabeticorum is a diagnosis that needs to
be remembered by the physicians and they must evaluate
the possibility of local infection of the soft tissue and bone
parts. Because of a self-limited course, usually painless,
no specific treatment or invasive diagnostic procedures
are required.
Referencias
- Kramer DW: Early warning signs of impending gangrene in diabetes mellitus. Med J Rec 1930; 132: 338-342.
- Taylor SP, Dunn K. Bullosis Diabeticorum. J Gen Intern Med. 2017 feb; 32(2): 220.
- Cantwell AR, Martz W: Idiopathic bullae in diabetics. Arch Dermatol 1967; 96: 42-44.
- Derighetti, M et al. Bullosis diabeticorum in a Newly Discovered Type 2 Diabetes mellitus. Dermatology 2000; 200: 366-b367.
- Gupta, V et al. Bullosis Diabeticorum: Rare Presentation in a Common Disease. Case Reports in Endocrinology. Volume 2014, Article ID 862912, 3 pages.
- Mota, A N C M, Nery N S, Barcaui C B. Caso para diagnóstico. An Bras Dermatol. 2013; 88(4): 652-654.
- Bernstein JE, Medenica M, Soltani K: Bullous eruption of diabetes mellitus. Arch Dermatol 1979; 116: 324-325.
- Bernstein JE, Levine LE, Medenica M: Reduced threshold to suctioninduced blister formation in insulin-dependent diabetics. J Am Acad Dermatol 1983; 8: 790-791.
- Toonstra J: Bullosis diabeticorum: Report of a case with review of literature. J Am Acad Dermatol 1985; 13: 799-805.
- Larsen K, Jensen T, Karlsmark T, Holstein PE. Incidence of bullosis diabeticorum-a controversial cause of chronic foot ulceration. Int Wound J 2008; 5: 591-596.
- Bello, F et al. 2 Cases of Bullosis Diabeticorum following Long-Distance Journeys by Road: A Report of 2 Cases. Case Reports in Endocrinology Volume 2012, Article ID 367218, 5 pages.
- Kurdi AT. Bullosis diabeticorum. Lancet. 2013 Nov 30; 382(9907): e31.